Abdominal actinomycosis
Description
Abdominal actinomycosis is a chronic disease caused by various types of actinomycetes. It is characterized by lesions of various body tissues and organs through the formation of dense infiltrates, subsequently causing the appearance of abscesses, fistulas or peculiar skin lesions.
What causes it?
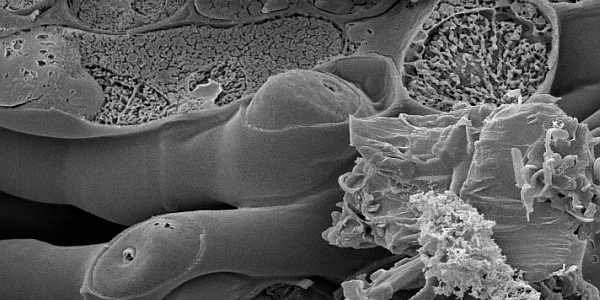
The pathogens are the radiating bacteria Actinomyces Israeli, which grow best in nutrient media by forming irregularly shaped colonies, often with radiating ends . Actinomycetes are sensitive to benzylpenicillin, streptomycin, tetracycline, chloramphenicol and erythromycin.
The radioactive bacteria are distributed in all countries. Their source is sick people and livestock. However, cases of human infection from another sick person or animal have not been described.
Actinomycetes can be found almost everywhere in nature – hay, straw, soil, etc. They are also often found in the mouth, tonsils and mucous membranes of the gastrointestinal tract in healthy people. Therefore, there are exogenous and endogenous ways to induce infection.
Pathogenesis
Most often, the disease is caused by an endogenous pathway. Radiant bacteria are mainly found in plants and can enter the human body from them and inhabit his mucous membranes as saprophytes.
The transition of actinomycetes from a saprophytic to a parasitic state contributes to inflammatory diseases of the oral mucosa, respiratory tract and gastrointestinal tract. An infectious granuloma forms at the site of the actinomycete infection, which grows and covers the surrounding tissues.
Abscesses are formed in it, which break and form fistulas. Skin damage is secondary in nature.
What are the symptoms?
The initial symptoms of the disease are usually vague and poorly expressed. They are most often manifested by fever, malaise, weakness and pain, which slowly and progressively increases.
The process of infection development resembles slowly progressing malignant tumor formations such as stomach cancer, of colon and rectum or the cervix. Large subcutaneous abscesses, extensive seals on the skin or fistulas in which the radioactive bacteria have been released can be observed and this is often the first characteristic sign of the disease.
Without effective treatment, radioactive bacteria can spread to nearby tissues or organs, including the liver, spleen, kidneys, fallopian tubes, ovaries, uterus, testicles, bladder, rectum, or abdominal wall.
Treatment of abdominal actinomycosis
The best results are achieved by a combination of etiotropic therapy with antibiotics and immunotherapy with actinolyzate. Large doses of benzylpenicillin 10,000,000 are most often prescribed. IU per day or more, which are infused intravenously for 1-1.5 months, subsequently switching to phenoxymethylpenicillin with a daily dose of 2-5 grams for 2-5 months.
For secondary purulent infection, most often with staphylococci or anaerobic bacteria, long courses of antibiotics from the dicloxacillin or tetracycline group are prescribed, and for anaerobic infections, metronidazole.
In immunotherapy, actinolyzate can be administered subcutaneously, intradermally, and also intramuscularly. 3 ml are injected subcutaneously and intramuscularly. actinolyzate 2 times a month.
Usually a 3 month course with 20-30 injections is prescribed. In case of abscess and empyema – accumulation of pus in a cavity in the body, surgical treatment is carried out – incision and drainage. In very large lesions of the lung tissue, lobectomy is sometimes resorted to.
Of the antibiotics, the most effective are tetracycline, followed by penicillin and less effective is erythromycin. Resistant to these medications strains of the radiant bacterium have not been detected.
p>
Without treatment, the prognosis is unfavorable. With abdominal actinomycosis, 50% of patients die, and with thoracic, all patients die. Cervical-facial-jaw actinomycosis is relatively mild.
All this determines the need for early diagnosis and the initiation of treatment before the development of severe anatomical damage. Given the risk of re-infection, recovered patients should be observed for a minimum of 6-12 months.



